Atherosclerotic Diseases of the Aorta
Copyright 2007
Ashley Davidoff MD
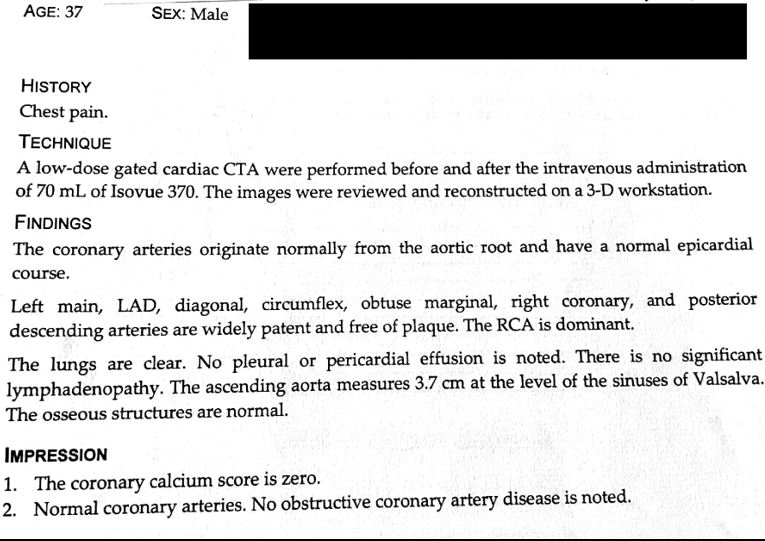
The most common disease of the aorta is atherosclerosis, a process in which lipid material, fibrous tissue, and calcium form deposits, called plaques, within the inner layer of the aortic wall (the intima). The earliest signs of atherosclerotic change are yellow fatty streaks in the intima Although it is an area not prone to atherosclerosis, these fatty streaks are first observed in the descending thoracic aorta adjacent to the departure of intercostal arteries (1) After age 20 years, atherosclerotic plaques are more extensive in the abdominal aorta than in any other area Aortic (true) aneurysms are thought to be caused by a variety of factors including atherosclerosis; the vast majority of aortic aneurysms are found in the infrarenal abdominal aorta (2) The ascending thoracic aorta is the area least prone to atherosclerosis Aortic dissections occur as a result of hypertension, and are formed after the intima of the aorta ruptures, leading to entry of blood into the aortic wall Initiating tears are most frequent in the ascending aorta, though the ascending aorta is not the most commonly involved portion of the aorta regarding dissecting aneurysms The proximal portion of the descending thoracic aorta is the second most common location of a primary intimal tear, but because most ascending aortic dissections extend to involve the descending portion, and because few primary tears in the descending aorta extend retrograde to the ascending aorta, the descending aorta is the most commonly involved portion of the aorta with dissecting aneurysms (3)
Pathogenesis
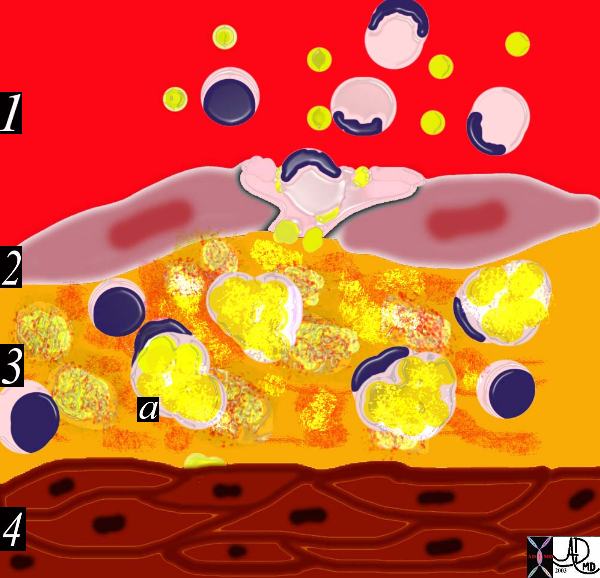
Atherosclerosis is a degenerative disorder of the intima of arteries. (occasionally affecting other structures in the cardiovascular system) chatracterised by accumulation of fatty and fibrous elements within the intima of the vessel wall. The multifactorial causes of atherosclerosis include age, sex, genetics, lifestyle and dietary factors. among many other unfolding factors. The recognizable “phases” of atherosclerosis include ; 1) breach of the endothelium (33792d) 2) migration of lipoproteins from the lumen into the intima. (33792d) 3) Formation of a lipoprotein-proteoglycan complex that traps the lipoprotein in the intima (33792e) 4) Migration of leukocytes from the lumen into the intima. (33792g) 5) Transformation of the monocytes into macrophages and phagocytosis of the fat complexes to form fat laden foamy macrophages. (33792h) 6) Migration of smooth muscle cells from the media into the intima and transformation into fibrocytes. A fibrous capsule around the fatty complex is formed. (33792i, 33801b) 7) Cell death and destruction with associated formation of dystrophic calcification. 8) Growth of the atheromatous complex with impingement on the lumen. (33801b) 9) Potential of the complex to rupture. (33801d) The progressive impingement on the lumen causes reduction of blood flow, usually manifesting clinically with angina when the lumen is reduced by 70% of its original size. Acute rupture of a plaque predisposes to superadded thrombosis and occlusion of the lumen. Acute myocardial infarction and death are complications of this event. The initial phase of endothelial injury has multifactorial contributing factors including hypertension, hemodynamic factors, hyperlipidemia, homocysteine, smoking, toxins, immune reactions, and viral disease. The result is a breach in the intima and migration of lipoproteins into the subendothelial layer. The lipoproteins and proteoglycans form a complex compound that traps the fat complex in the subepithelial layer. The next phase heralds the migration of leukocytes and platelets into the subendothelial layer. The monocytes, phagocytose the lipoprotein-proteoglycan complex forming the lipid laden foamy histiocytes. These macrophages can apparently repllicate. At this stage the macroscopic appearance is the well known “fatty streak”. The next phase of atherosclerosis occurs following smooth muscle proliferation and migration from the media into the evolving plaque. Smooth muscle also undergoes apoptosis and death. The vascular smooth muscle produces the extracellular matrix has major contribution to the atheromatous lesion. Interstitial collagens (types I and III) and proteoglycans such and elastin fibers also accumulate in atherosclerotic plaques. Accumulation of cholesterol and cholesterol esters occur. Smooth muscle migrates from the media into the intima and transform into fibrous elements both within the lesion as well superficial to the lesion forming a fibrous plaque. The monocytes and macrophages ingest the fat and foamy fat laden macrophages result. An inflammatory reaction evolves. Continued accumulation of lipid, macrophages, foamy cells, extracellular matrix result in a fibrofatty complex that grows in size over time. As it enlarges it bulges and thins the intima and eventually erodes the surface. As the disease progresses, cell death within the plaque results, and dystrophic calcification follows.
Ashley Davidoff MD
THECOMMONVEIN.netNormal

This image shows normal circulating lipoproteins in the circulation. The intima is intact and the wall is normal. Note the normal presence of lipoprotein molecules in the lumen. Courtesy Ashley Davidoff MD. 33789 code heart artery wall histology normal drawing pathogenesis atherosclerosis atheroma Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net

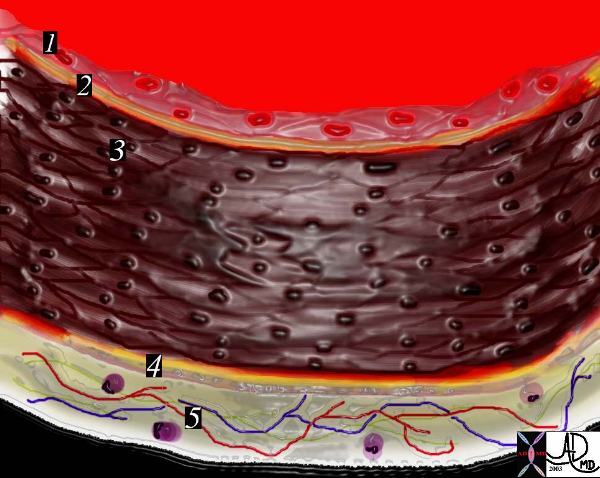
In the early stages of atherosclerosis there is intimal injury and a breach in the endothelium. 33790 artery lumen intima endothelium internal elastic membrane media muscularis muscular layer external elastic membrane adventitia vavsa vasorum capillaries circulating phospholipids intimal injury normal anatomy histology drawing art Courtesy Ashley Davidoff MD
THECOMMONVEIN.net

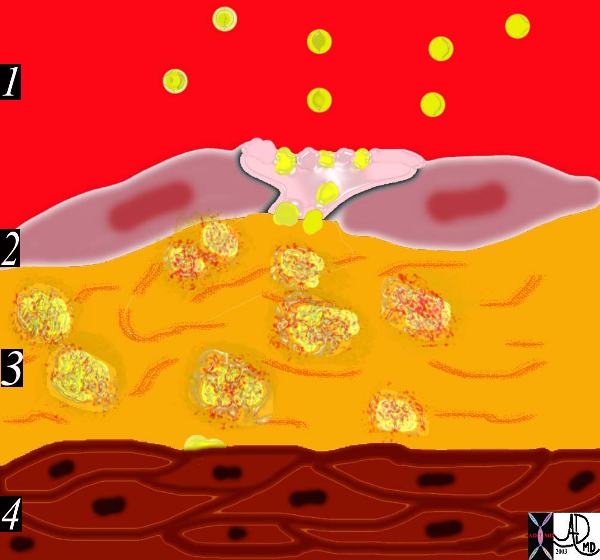
The circulating lipoproteins enter a breached endothelium (2) and enter the subendothelial layer of supporting connective tissue within which are linear starands of proteoglycan. (3). At this stage the media (4) is quiescent. Courtesy Ashley Davidoff MD 33792d code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
This diagram shows the yellow spheroidal lipoproteins traversing the injured epithelium (2) from the lumen (red) and binding to the linear shaped proteoglycan molecules in the intimal layer. (3) In essence the lipoprotein is “captured”, because it has been altered structurally and is unable to return to the circulation.
Courtesy Ashley Davidoff MD. 33792e code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
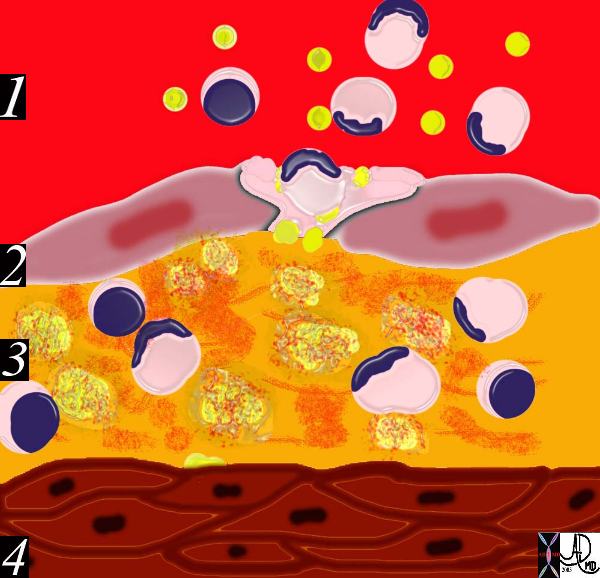
The diagram shows an evolving atheromatous plaque with inflammatory cells, monocytes, and lymphocytes infiltrating the intima which contains the lipoprotein- proteoglycan complex, extracellular lipid , and cholesterol crystals. 33792g Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
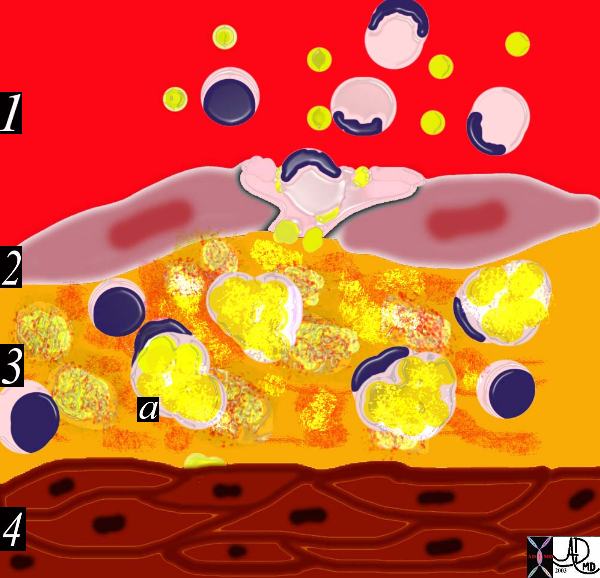
This drawing shows migration of the monocytes into the intima. These monocytes transform into macrophages in the intima and phagocytose the lipid products to become lipid laden foamy cells. The macroscopic correlate at this stage is the fatty streak. Courtesy Ashley Davidoff MD 33792h . code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net

This diagram shows the reaction of the smooth muscle cells (b) to the formation of foam cells (a) in the subendothelial layer of the intima. The smooth muscle cells migrate from the muscular layer (4) into the intima. Here they undergo dedifferentiation into fibrocytes. 33792i
endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
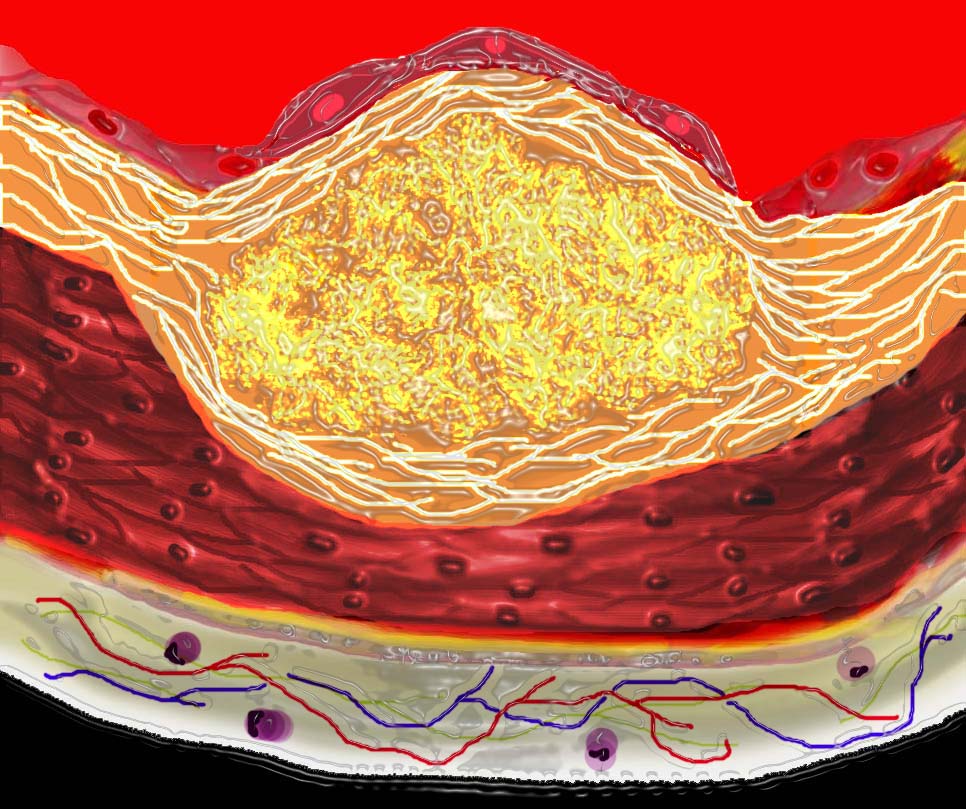
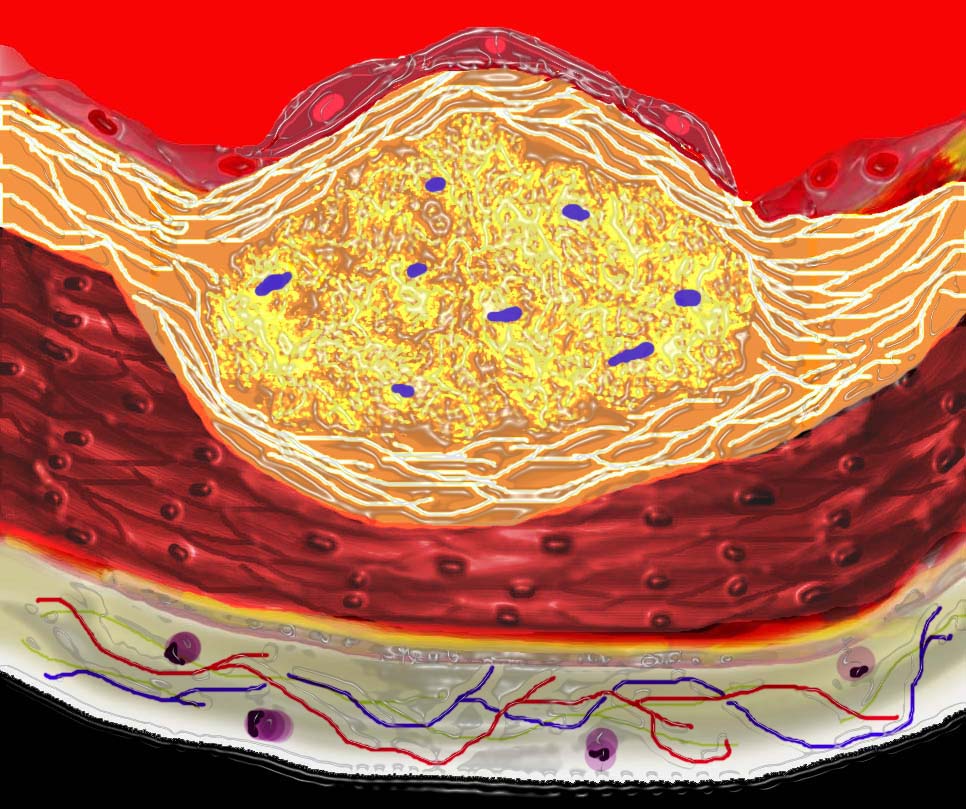
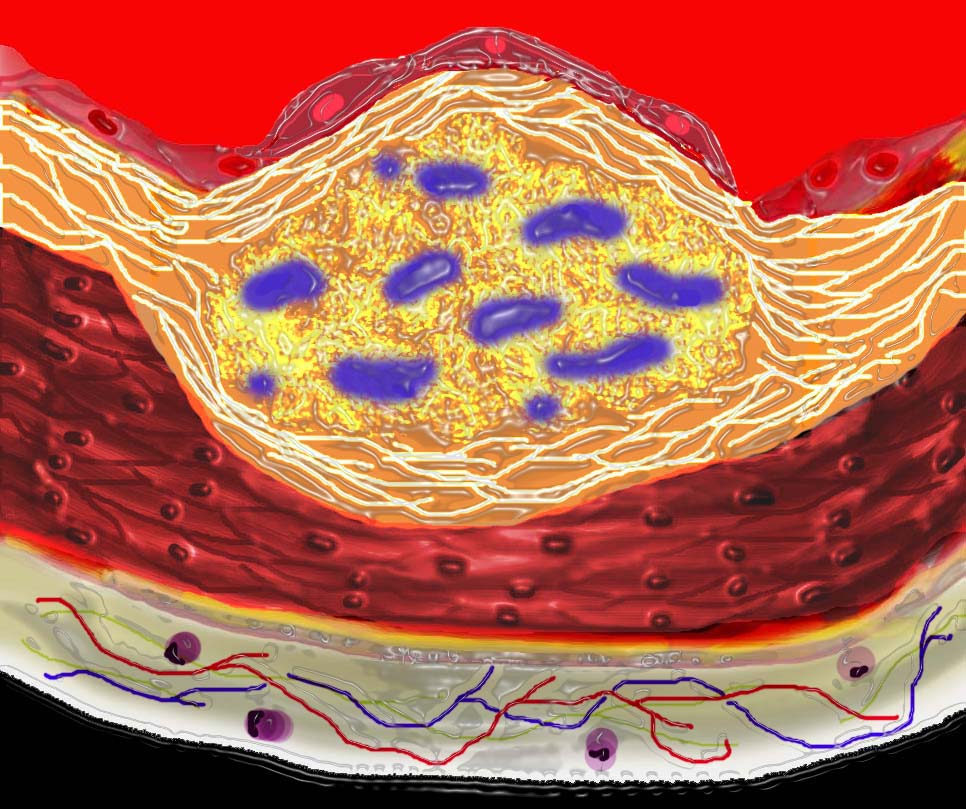
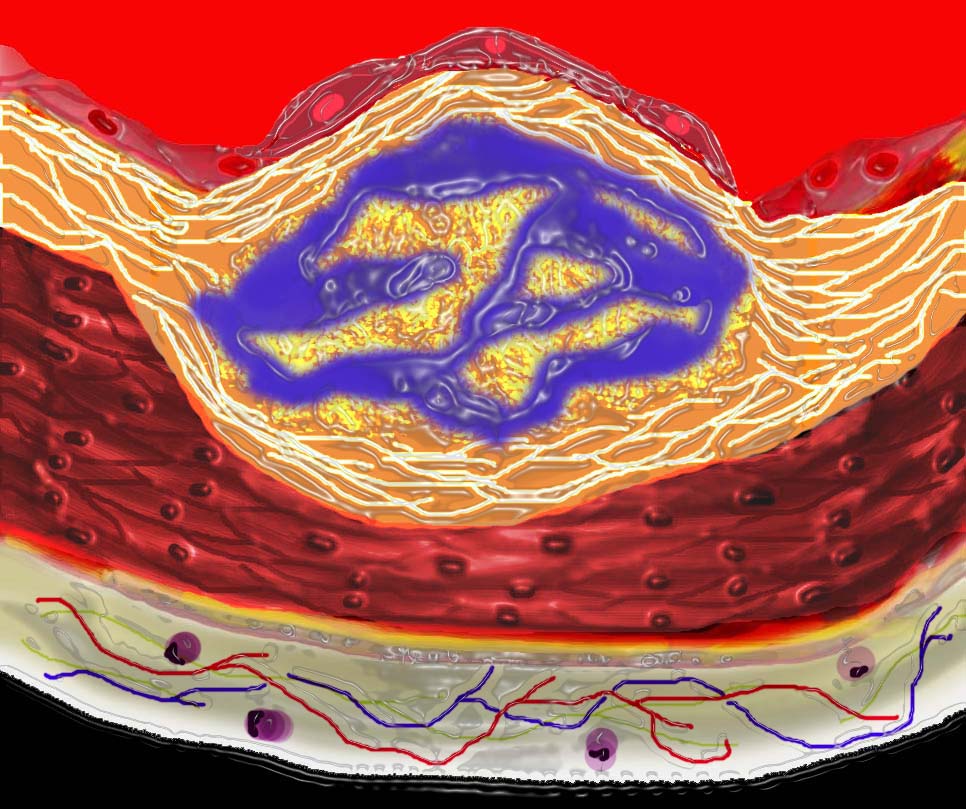
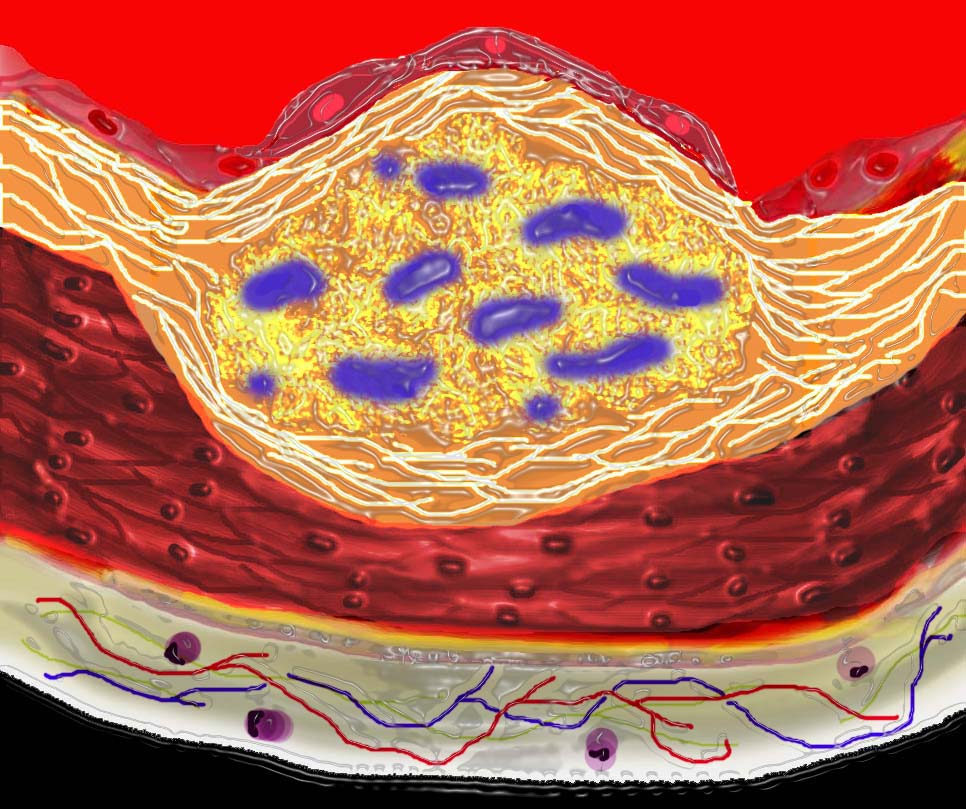
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which is bulging both toward the media and toward the lumen. There is a central core of fat and necrotic debris, surrounded by fibrous elements which give the plaque its hardness to the feel. The accumulation of fibrous tissue heralds an advanced atherosclerotic lesion. 33801b01
Courtesy Ashley Davidoff MD. code heart artery atherosclerosis Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net

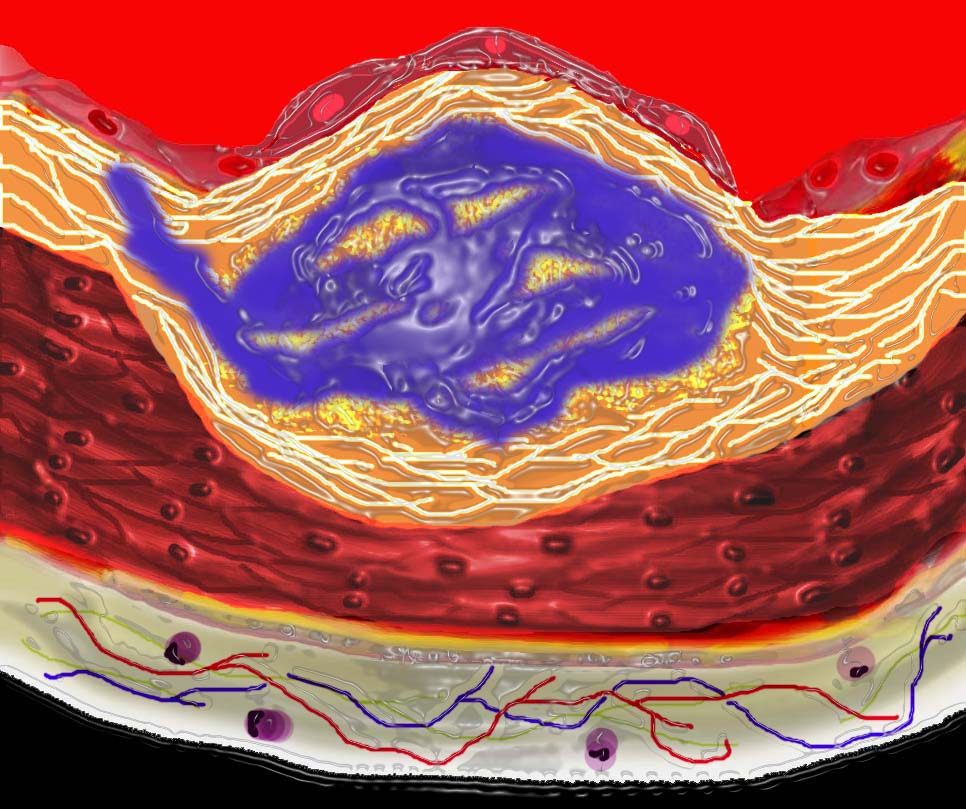
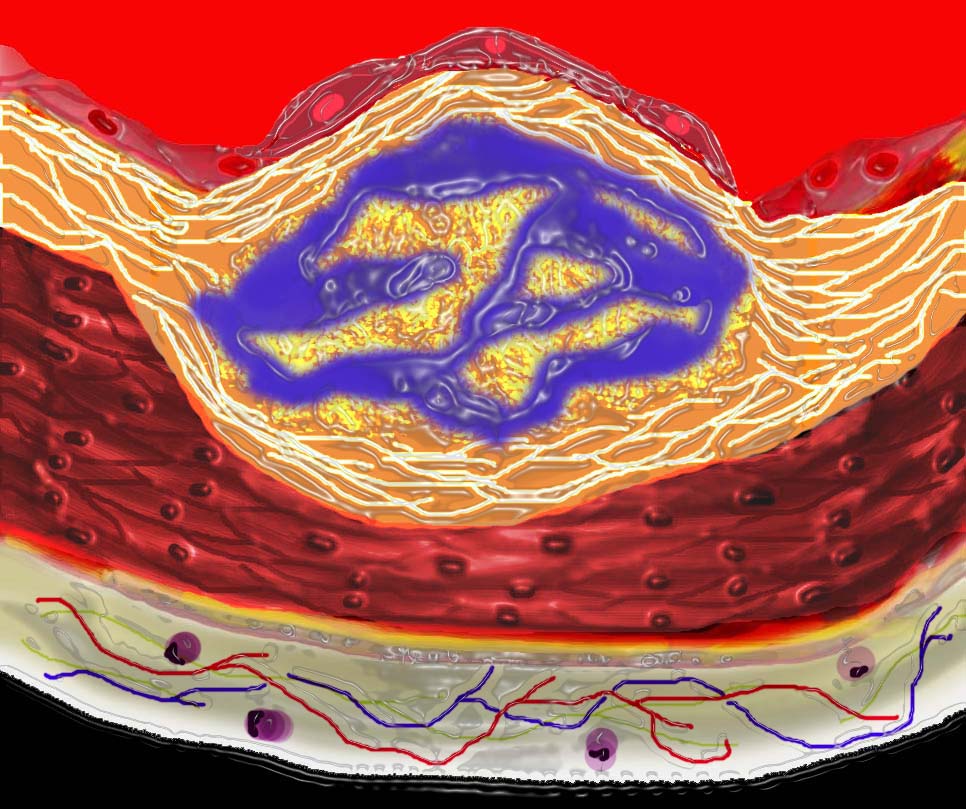
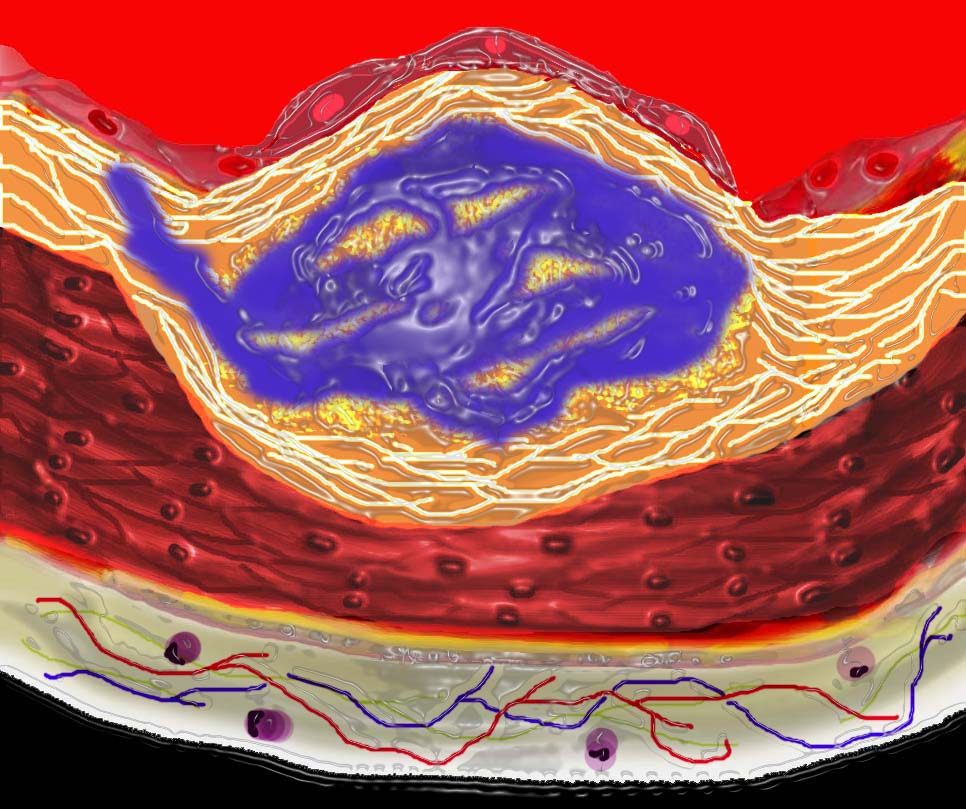
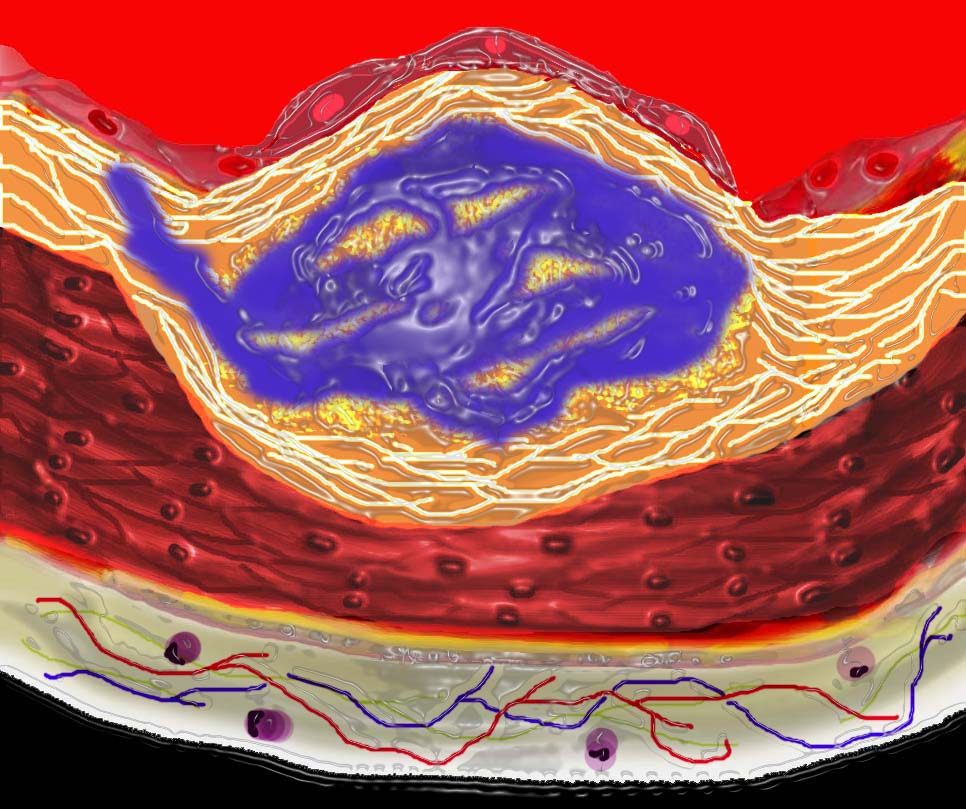
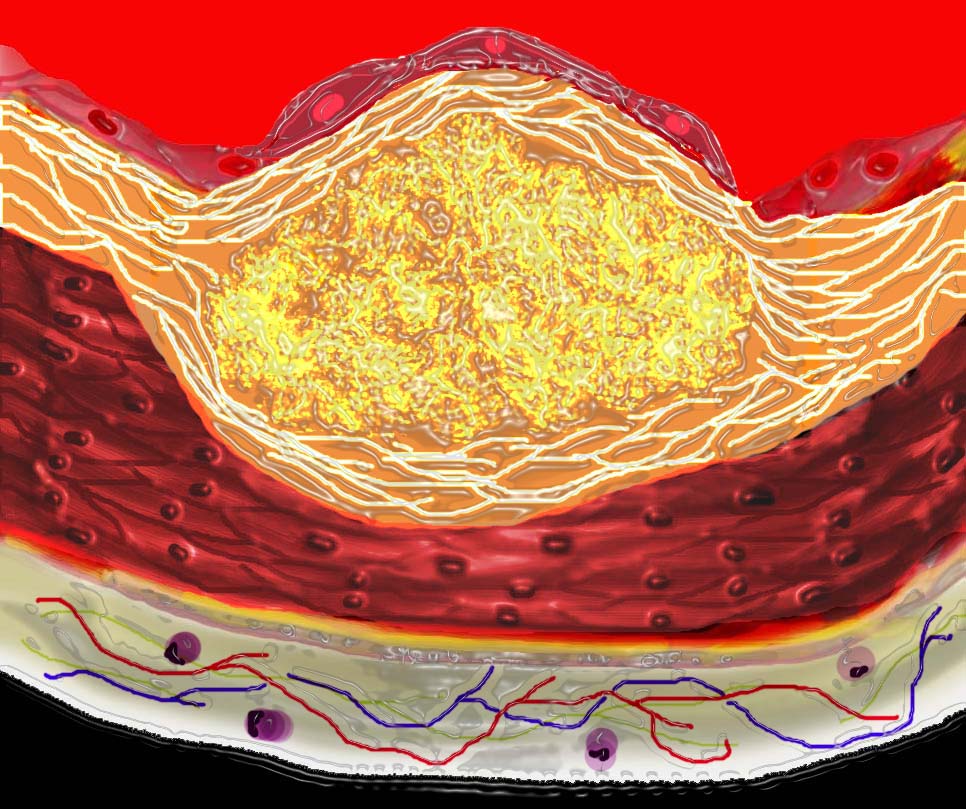
This diagram shows denudation of the endothelial layer with exposure and rupture of the contents of the atherosclerotic plaque in volcanic fashion into the lumen. This event is catastrophic and can result in acute thrombosis and may even be a fatal event. 33801d01 Courtesy Ashley Davidoff MD. code heart artery atherosclerosis atheroma vulnerable plaque drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
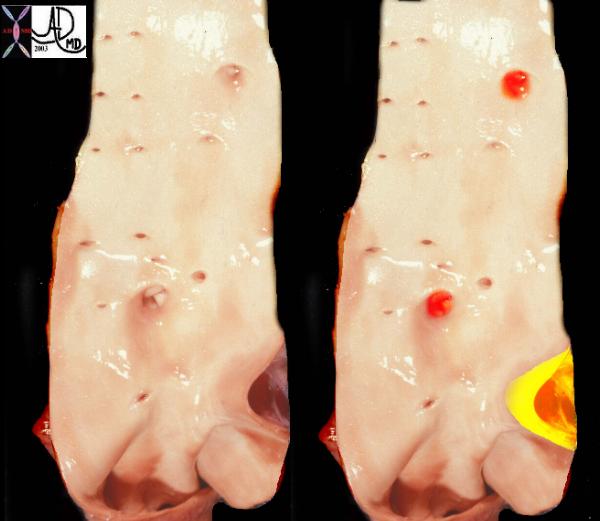
This is a post mortem specimen of the aorta of a patient with pulmonary atresia and bronchial collaterals. Overlaid in red are the enlarged orifices of the origins of the bronchial arteries. In yellow is the entrance of the PDA (patent ductus arteriosus) to the aorta Note in addition the normal appearing shiny appearance of the neonatal intima. Courtesy Ashley Davidoff MD 32628c a79-8
THECOMMONVEIN.net
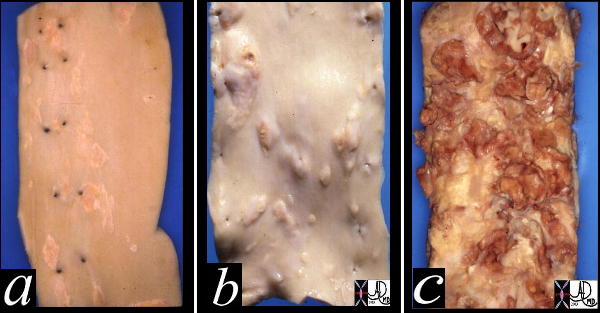
This image shows three pathological specimens of the aorta. In the first image minimally raised fatty streaks are noted. (a). In image b, the fibrous capsule causes raised fibrofatty nodules, while in c, there gas been rupture of the plaques, with friable atheromatous plaques abound. Courtesy Henri Cuenoid MD 13420c CVS artery aorta atheroscleosis atheroma fatty streaks fibro
THECOMMONVEIN.net
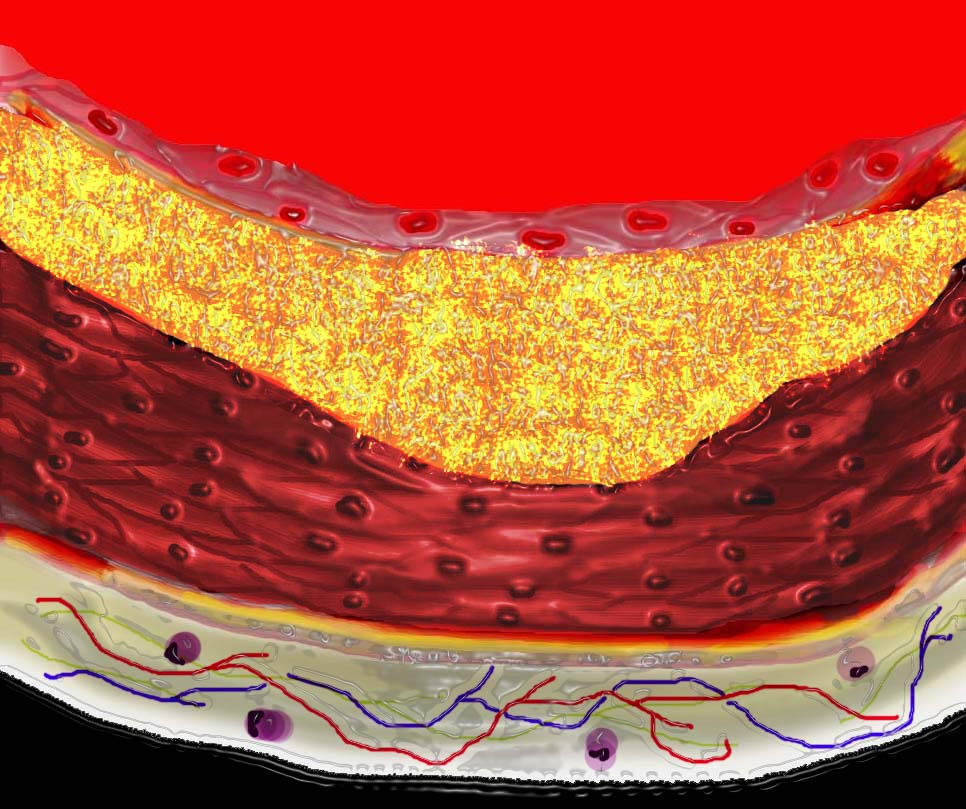
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which at first bulges toward the media or muscular layer. 33801a Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
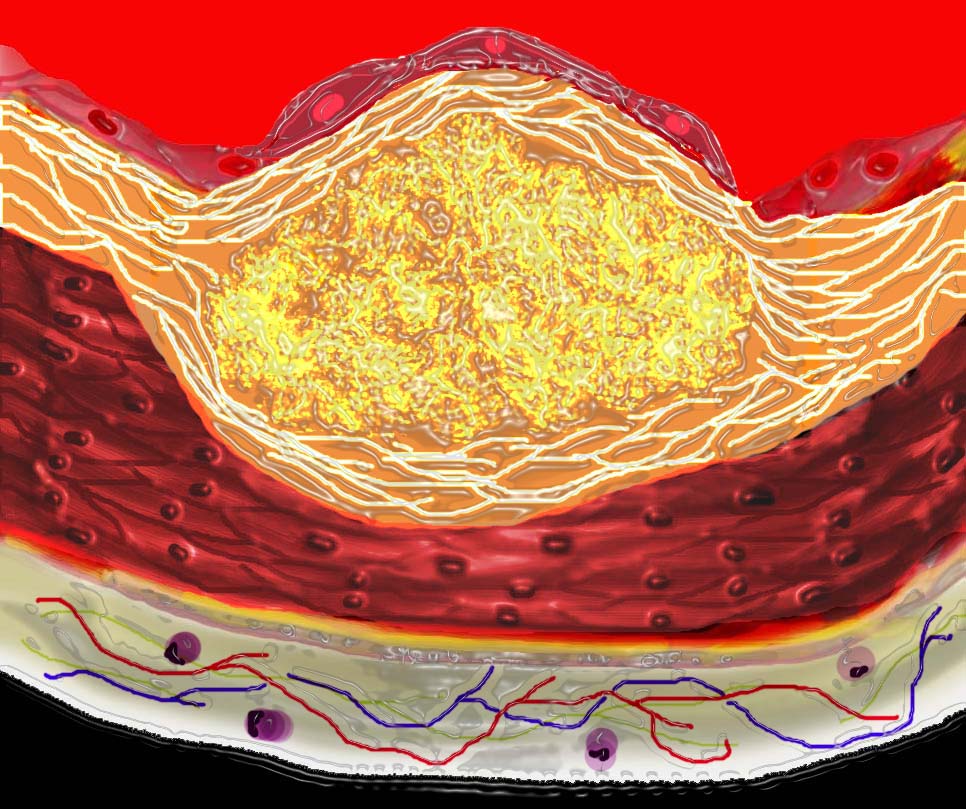
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which is bulging both toward the media and toward the lumen. There is a central core of fat and necrotic debris, surrounded by fibrous elements which give the plaque its hardness to the feel. The accumulation of fibrous tissue heralds an advanced atherosclerotic lesion. 33801b01
Courtesy Ashley Davidoff MD. code heart artery atherosclerosis Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net

This diagram shows denudation of the endothelial layer with exposure and rupture of the contents of the atherosclerotic plaque in volcanic fashion into the lumen. This event is catastrophic and can result in acute thrombosis and may even be a fatal event. 33801d01 Courtesy Ashley Davidoff MD. code heart artery atherosclerosis atheroma vulnerable plaque drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
Why is it Important to Understand
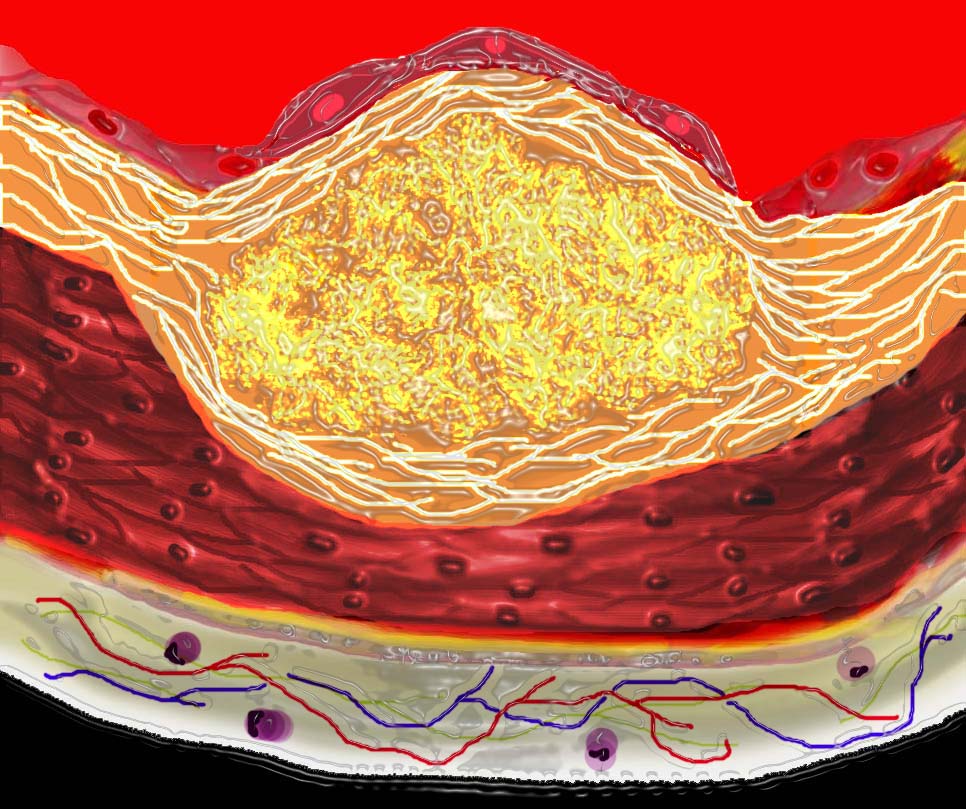
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which is bulging both toward the media and toward the lumen. There is a central core of fat and necrotic debris, surrounded by fibrous elements which give the plaque its hardness to the feel. The accumulation of fibrous tissue heralds an advanced atherosclerotic lesion. 33801b01
Courtesy Ashley Davidoff MD. code heart artery atherosclerosis Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
Stenotic Disease
Ashley Davidoff MD
THECOMMONVEIN.net
Ashley Davidoff MD
THECOMMONVEIN.net
The Fear – The Vulnerable Plaque

This diagram shows denudation of the endothelial layer with exposure and rupture of the contents of the atherosclerotic plaque in volcanic fashion into the lumen. This event is catastrophic and can result in acute thrombosis and may even be a fatal event. 33801d01 Courtesy Ashley Davidoff MD. code heart artery atherosclerosis atheroma vulnerable plaque drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
The Cutting Edge and the Holy Grail
Ashley Davidoff MD
Ashley Davidoff
The CommonVein.net

Filet view
Ashley Davidoff
Evaluating the Chemical Makeup of the Wall of the Arteries
Wall
Links and References
Acute Aortic Syndrome
Atherosclerosis Pathogenesis
Ulcerated Plaque
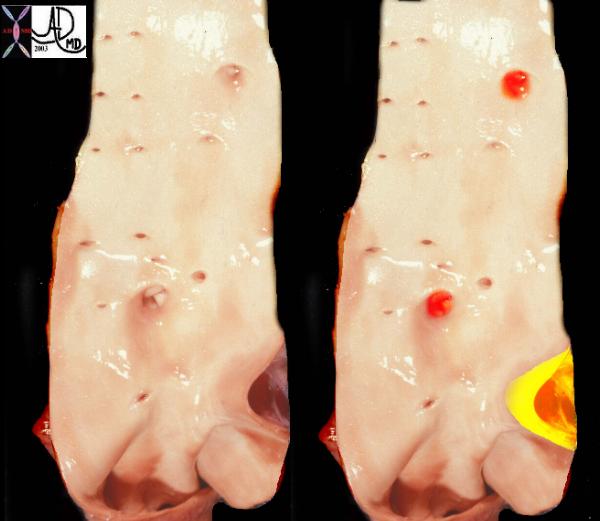
This is a post mortem specimen of the aorta of a patient with pulmonary atresia and bronchial collaterals. Overlaid in red are the enlarged orifices of the origins of the bronchial arteries. In yellow is the entrance of the PDA (patent ductus arteriosus) to the aorta Note in addition the normal appearing shiny appearance of the neonatal intima. Courtesy Ashley Davidoff MD
Ashley Davidoff MD THECOMMONVEIN.net 32628c

In the early stages of atherosclerosis there is intimal injury and a breach in the endothelium. key Key Words artery lumen intima endothelium internal elastic membrane media muscularis muscular layer external elastic membrane adventitia vasa vasorum capillaries circulating phospholipids intimal injury normal anatomy histology drawing art Courtesy Ashley Davidoff MD
Ashley Davidoff THECOMMONVEIN.net 33790

The circulating lipoproteins enter a breached endothelium (2) and enter the subendothelial layer of supporting connective tissue within which are linear starands of proteoglycan. (3). At this stage the media (4) is quiescent. Courtesy Ashley Davidoff MD 33792d code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net 33792d
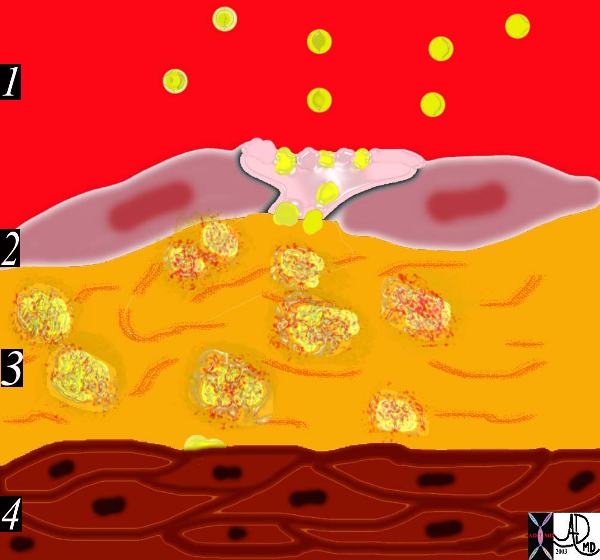
This diagram shows the yellow spheroidal lipoproteins traversing the injured epithelium (2) from the lumen (red) and binding to the linear shaped proteoglycan molecules in the intimal layer. (3) In essence the lipoprotein is “captured”, because it has been altered structurally and is unable to return to the circulation.
Key Words code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Courtesy Ashley Davidoff MD. 33792e Davidoff art
THECOMMONVEIN.net 33792e
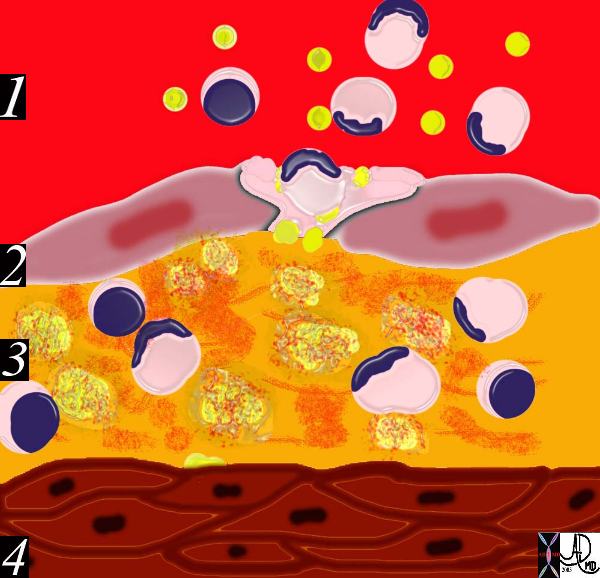
The diagram shows an evolving atheromatous plaque with inflammatory cells, monocytes, and lymphocytes infiltrating the intima which contains the lipoprotein- proteoglycan complex, extracellular lipid , and cholesterol crystals. 33792g Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
This drawing shows migration of the monocytes into the intima. These monocytes transform into macrophages in the intima and phagocytose the lipid products to become lipid laden foamy cells. The macroscopic correlate at this stage is the fatty streak. Courtesy Ashley Davidoff MD 33792h . code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net

This diagram shows the reaction of the smooth muscle cells (b) to the formation of foam cells (a) in the subendothelial layer of the intima. The smooth muscle cells migrate from the muscular layer (4) into the intima. Here they undergo dedifferentiation into fibrocytes. 33792i
endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
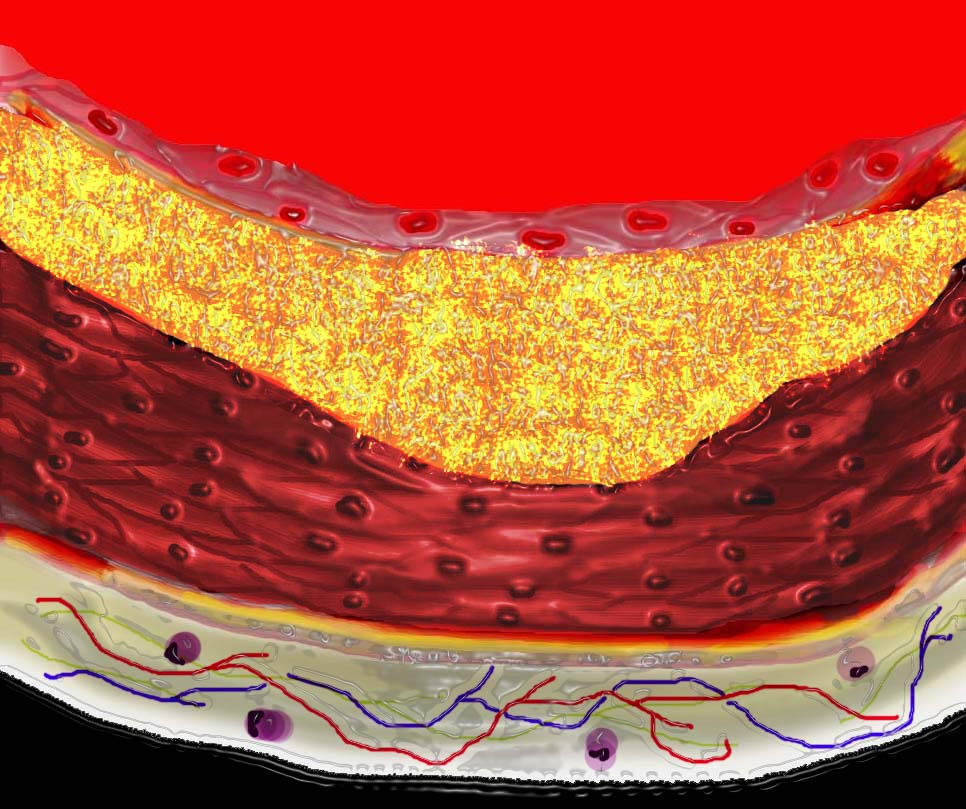
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which at first bulges toward the media or muscular layer. 33801a Courtesy Ashley Davidoff MD. code heart artery intima endothelium histopathology pathogenesis atherosclerosis atheroma drawing Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
The diagram shows the atherosclerotic lesion in the subepithelial layer of the intima which is bulging both toward the media and toward the lumen. There is a central core of fat and necrotic debris, surrounded by fibrous elements which give the plaque its hardness to the feel. The accumulation of fibrous tissue heralds an advanced atherosclerotic lesion. 33801b01
Courtesy Ashley Davidoff MD. code heart artery atherosclerosis Davidoff art
Ashley Davidoff MD
THECOMMONVEIN.net
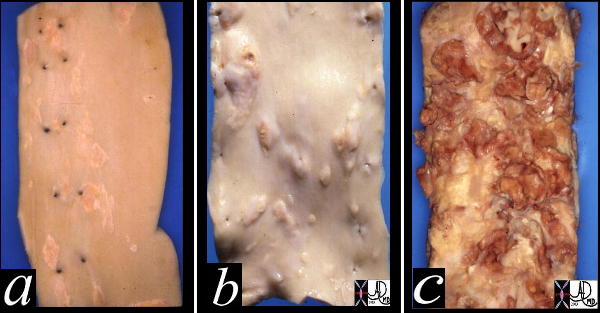
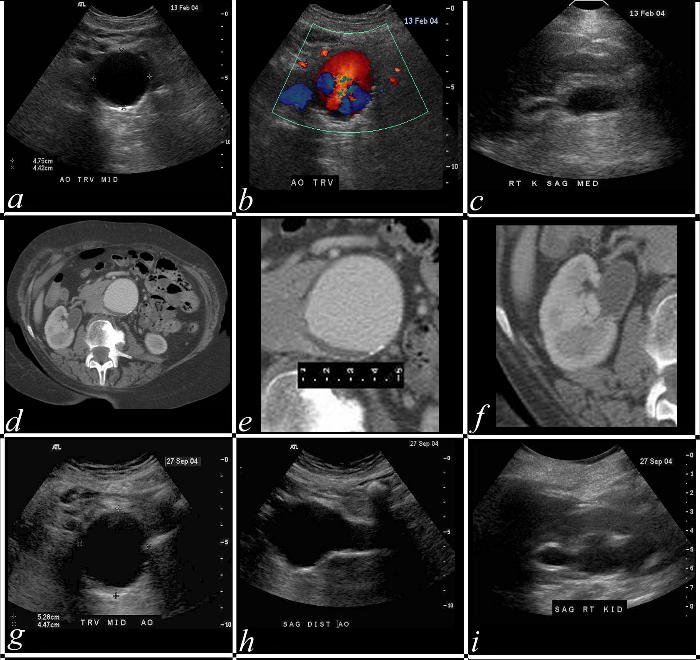
This image shows three pathological specimens of the aorta. In the first image minimally raised fatty streaks are noted. (a). In image b, the fibrous capsule causes raised fibrofatty nodules, while in c, there gas been rupture of the plaques, with friable atheromatous plaques abound. Courtesy Henri Cuenoid MD 13420c CVS artery aorta atheroscleosis atheroma fatty streaks fibro
THECOMMONVEIN.net
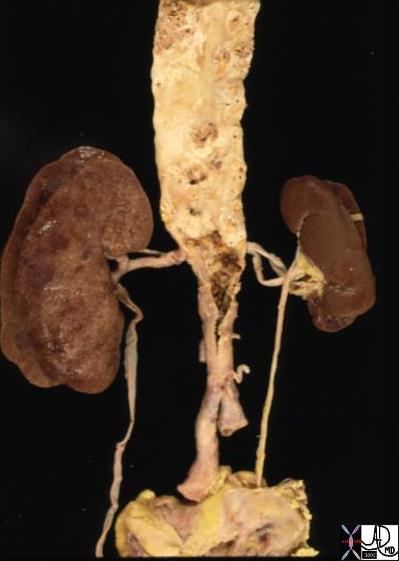
key words aorta abdomen iliac artery fx atherosclerosis kidney fx small dx RAS renal artery stenosis gross pathology Courtesy Ashley Davidoff MD THECOMMONVEIN.net 13417
Atherosclerosis of the Aortic Wall |
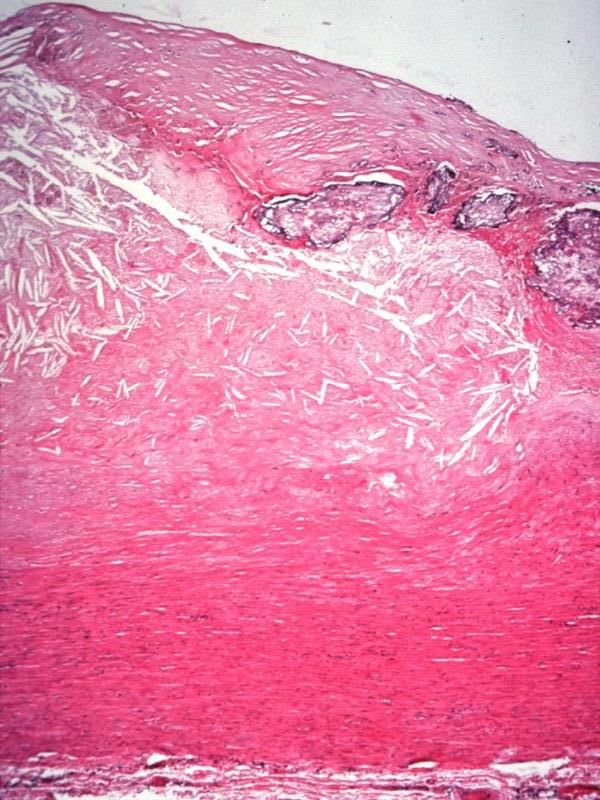
| 13316 13314 13313 aorta aortic wall elastic layer intima plaque complex lesion atherosclerosis atheroma complex lesion histopathlogy Courtesy Dr Isabelle Joris |
Normal and Severe Atherosclerosis |
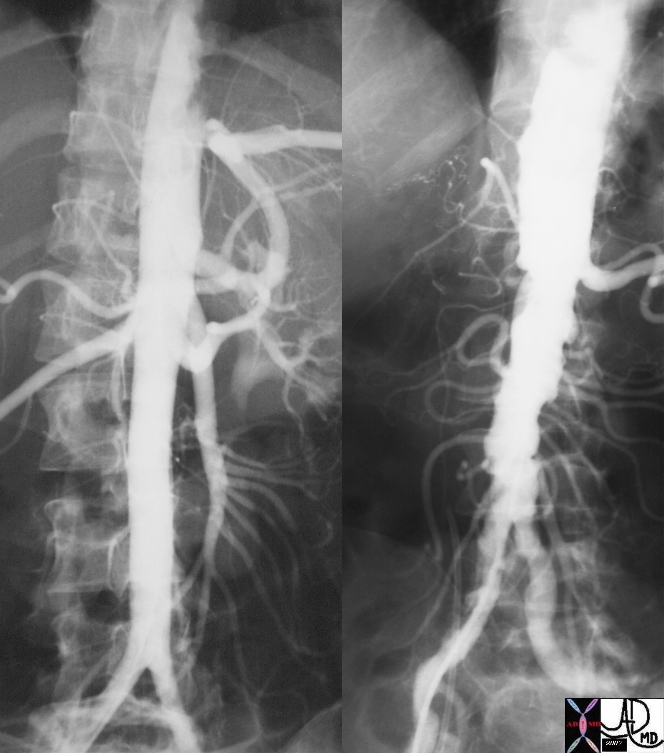
| 18485c01 aorta artery hepatic artery renal artery splenic artery superior mesenteric artery SMA kidney severe atheroscleroris atheroma occluded renal artery spleen liver normal anatomy angiogram angiography Davidoff MD |
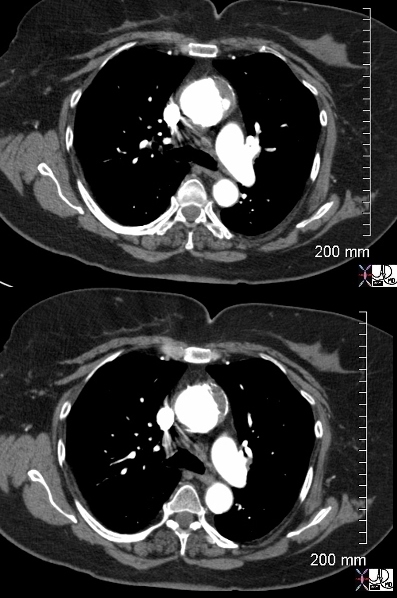
key words ascending aorta fx ulcer mural hematoma dx penetrating ulcer acute aortic syndrome CTscan Ashley Davidoff MD TheCommonvein.net 47792c01b
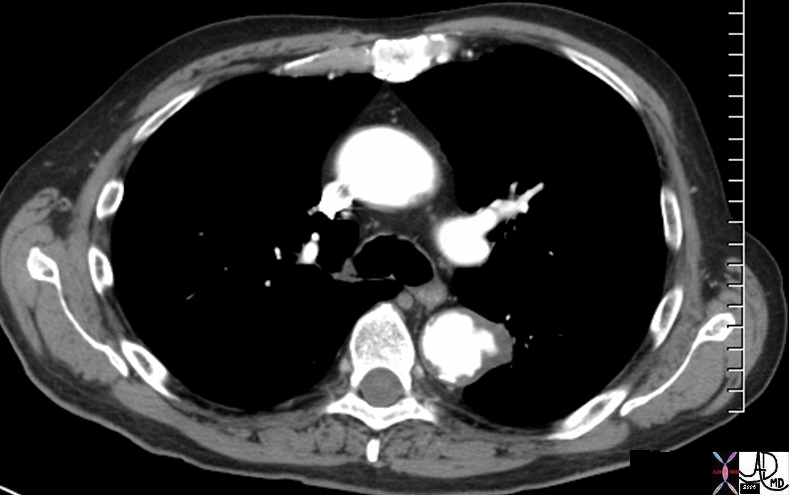
Penetrating ulcer in the descending descending thoracic aorta key words fx aortic ulcer fx atherosclerosis atheroma fx penetrating ulcer
acute aortic syndrome CTscan
Courtesy Ashley Davidoff MD TheCommonvein.net 48363
Penetrating ulcer in the descending descending thoracic aorta (bright red ) with overlying hematoma (maroon) key words fx aortic ulcer fx atherosclerosis atheroma fx penetrating ulcer
acute aortic syndrome CTscan
48363
Courtesy Ashley Davidoff MD TheCommonVein.net
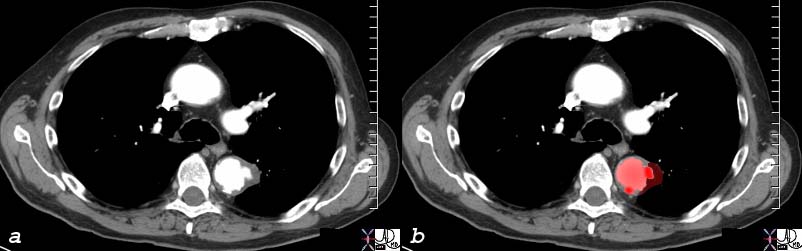
Pathogenesis of Penetrating Diseases of the Aorta and Acute Aortic Syndrome |
| 42409c01.800 aorta artery atherosclerosis atheroma acute aortic syndrome a aortic ulcer b = acute mural hematoma c = acute mural hematoma large d = focal dissection e penetrating ulcer f rupture histology histopathology Davidoff art pathogenesis Courtesy Ashley Davidoff MD |
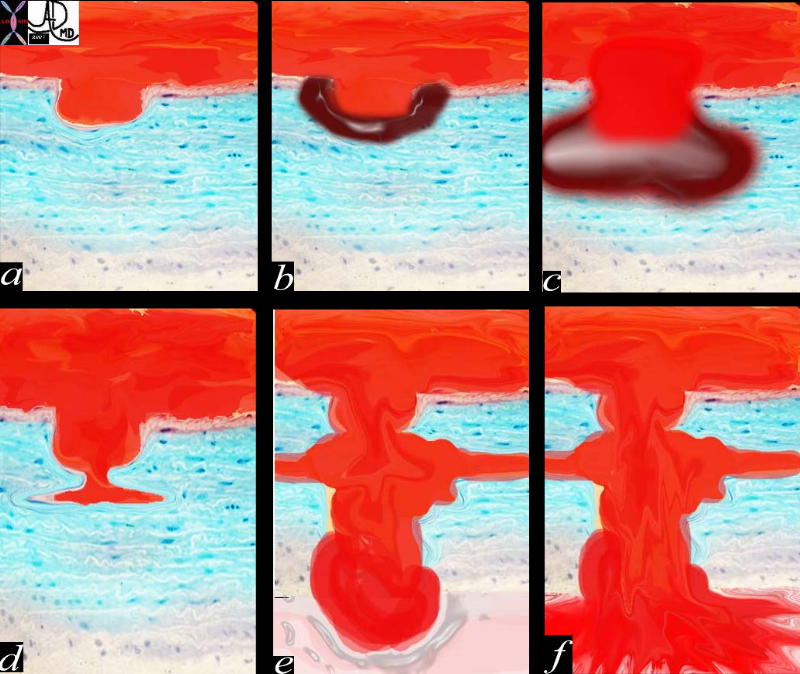
Growth Rate |
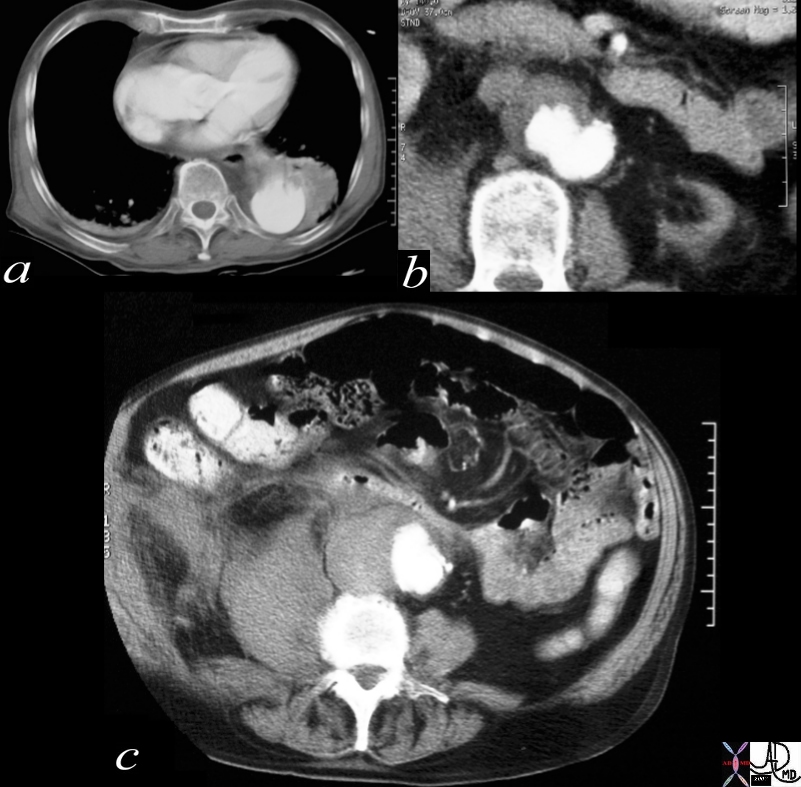
| This seriesof images spans the follow up of an infrarenal AAA first evaluated in February in 204 by US, (a,b,c) and CT (d,e,f) followed by a repeat US in September 2004 – 6 months later. The rapidity of growth from a transverse diameter of 4.8cms (a) to 5.3 cms (d) suggest rapid growth of the saccular aneurysm and in and of itself would warrant repair. In addition the presence of advancing hydronephrosis (c,i) would raise the possibility of perianeurysmal fibrosis with secondary obstruction probaly requiring surgical release and preferable treatment with open repair. Courtesy Ashley Davidoff MD 37245c code CVS aorta abdomen AAA infrarenal saccular hydronephrosis |
Aneurysm of the Abdominal Aorta |
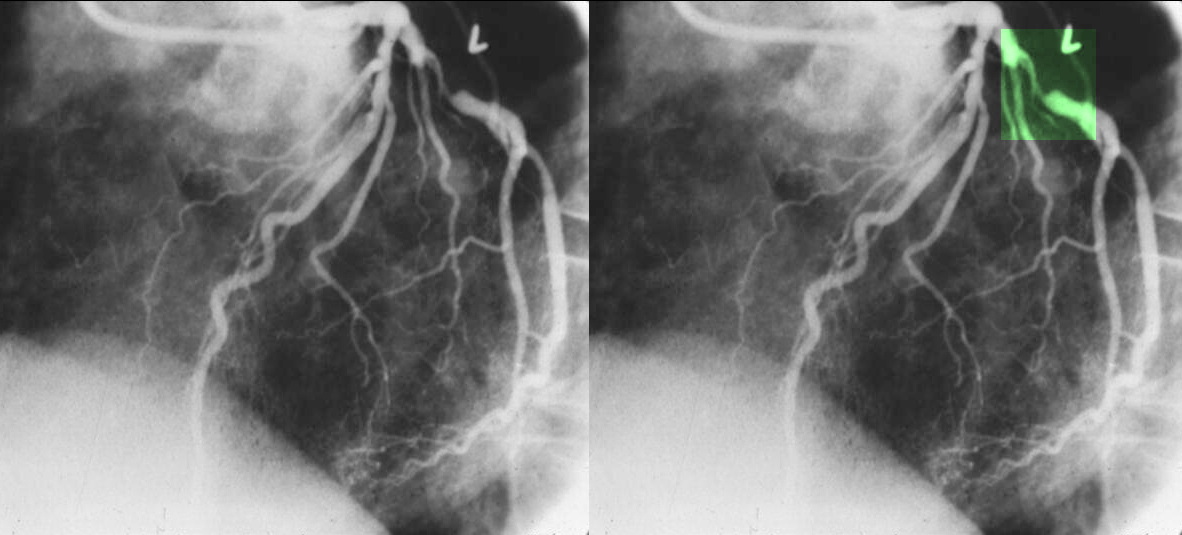
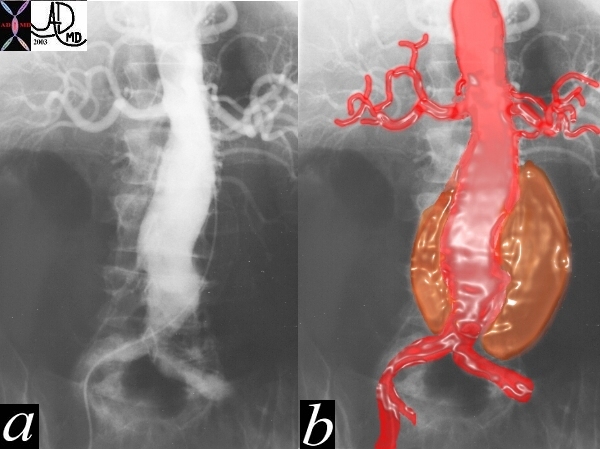
| This angiogram of the abdominal aorta shows a widened infrarenal aorta. At first glance the lumen of the aorta appears normal, but a faint curvilinar calcification of the true wall can be seen to the patients left in the first image. The second image (b) reveals the true size of the aneurysm. Courtesy Ashley Davidoff MD 22734 cW02 codeCVS aorta artery abdomen aneurysm AAA |
Penetrating Ulcer with Rupture |
| 17529c01 artery descending thoracic aorta abdominal aorta dx rupture pseudoaneumysm ulcerating plaque mural hematoma ruptured through aortic wall hemorrhage hematoma retroperitoneum CTscan Courtesy Ashley DAvidoff MD Ashley Davidoff MD |

Atherosclerotic Occlusion of the Aorta |
| 14646.803 aorta kidney size hypertrophy atrophy artery superior mesenteric artery arc of Drummond IMA inferior mesenteric artery collaterals renovascular disease occluded aorta internal iliac artery fx occluded occlusion small compensatory hypertrophy collaterals MRA MRIscan Davidoff MD |
Links and References