| Aortic Regurgitation
The Common Vein Copyright 2007 Ashley Davidoff MD Jessica Humphries Definition Aortic regurgitation is a circulatory disease characterized by the regurgitation, or backflow, of blood into the left ventricle of the heart. The primary cause of aortic regurgitation is intrinsic leaflet disease or annuloaortic ecstasia, which render the aortic leaflets incompetent. The result of this disease is regurgitation of blood into the left ventricle and a “water-hammer” pulse, which is an early diastolic murmur. The most commonly used diagnostic procedure for aortic regurgitation is echocardiography. This disease is usually treated with surgical replacement of the leaflets. Cause Aortic regurgitation is a circulatory disorder caused by incompetent aortic leaflets which fail to coapt during diastole allowing aortic blood to regurgitate into the LV causing overload on the left ventricle. Incompetence of the leaflets may result from intrinsic leaflet disease or due to ectasia of the annulus and aortic root. Leaflet disease includes congenital bicuspid valve, rheumatic disease, bacterial endocarditis, and myxomatous degeneration. Diseases that bay cause root aortic disease include Marfan’s syndrome, aortic dissection, traumatic laceration, ankylosing spondylitis, syphilitic aortitis, rheumatoid arthritis, Reiter’s disease. Result Diagnosis The Austin Flint murmur is the classical clinical situation that links the mitral aortic complex anatomically and physiologically as well as clinically. An Austin Flint murmur is a mid-diastolic, low-pitched rumbling heard at the ape caused by aortic regurgitant jet effect on the anterior leaflet of the mitral valve. The vibration of the anterior mitral leaflet occurs as it is buffetted simultaneously by the blood jets from the left atrium and the aortic regurgitant jet. Onset, duration, and termination of the Austin Flint murmur are related to the amount of LV volume overload and the end-diastolic pressure in the LV chamber. In the most severe form of increased end-diastolic pressure, the murmur is heard in early to mid diastole.
Clinical Clinically the disease is characterised by a “water-hammer” pulse, an early diastolic murmur which may also affect the mitral valve with early closure and a mid diastolic murmur called the Austin Flint murmur. The left ventricle is dilated. Imaging Imaging is best done using echocardiography which can identify and assess the severity of regurgitant flow with color doppler.
|
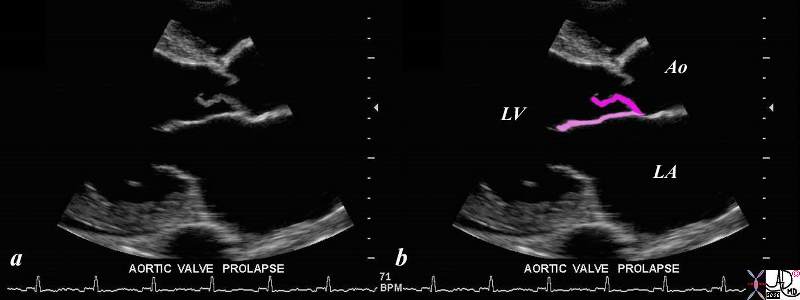
This gray scale echo of the heart showing a right parasternal long-axis left ventricular outflow view, and demonstrating prolapse of the aortic valve. The patient has a diagnosis of aortic regurgitation. The regurgitant jet of the aortic incompetence created by the prolapsing valve causes the mitral leaflet to flutter.
Ashley Davidoff TheCommonVein.net 33124
keywords cardiac heart echo AOV prolapse MV imaging echo 33124c02.8s
Treatment
Treatment is surgical replacement when indicated by clinical severity.
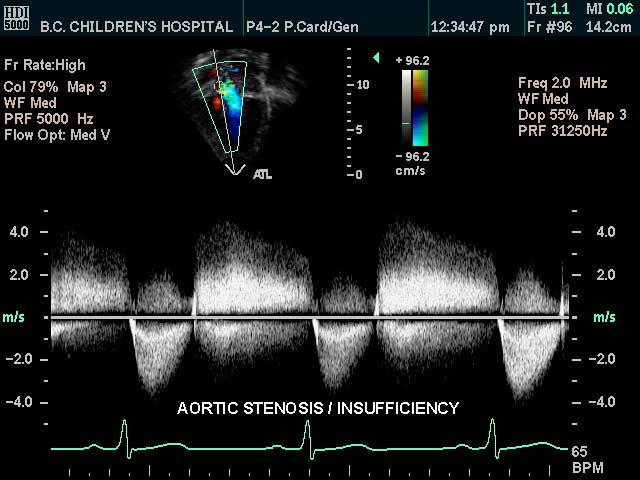 Aortic Stenosis and Insufficiency
Aortic Stenosis and Insufficiency