Structural Principles
The Common Vein Copyright 2007
The aorta’s structure conveys and relates to the basic mechanisms of tubular blood flow. Considering the aorta’s geometry in comparison to that of a straight cylindrical tube, the maintenance of laminar aortic blood flow in the presence of a180 degree turn, from ascending aorta to descending aorta is a remarkable accomplishment. . Blood flowing through the aorta experiences collisions with the curving elastic walls, and gradual tapering in its pathway as well as the presenc of branching vessels each with varying resistance —all of which are guided by the forces of pressure, governed by the rhythmical pumping of the heart, and the ovrall peripheral resistance .
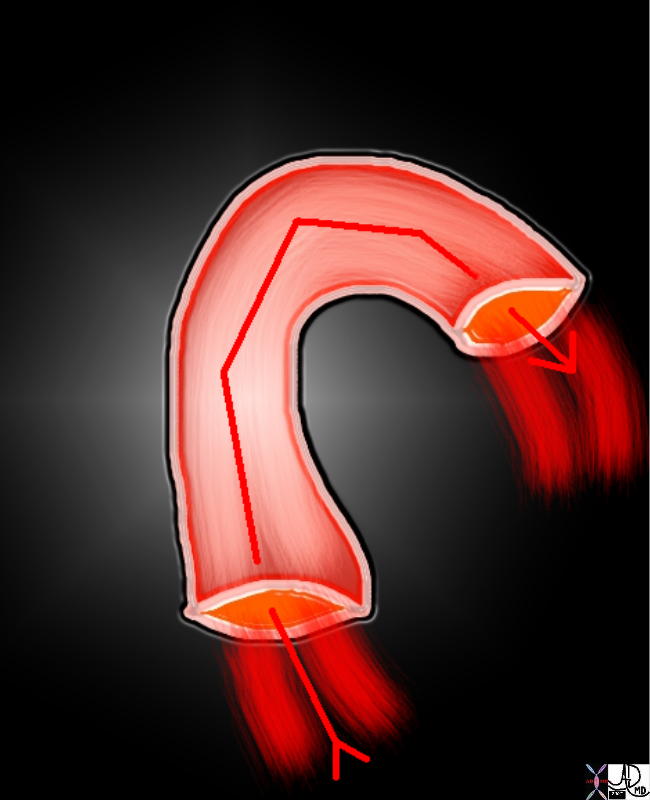 Gradual 180 degree turn Gradual 180 degree turn |
| The aorta is curved in shape and elastic in nature while blood is not a simple fluid and hence special circumstances exist
72835.800 aorta flow principles structure laminar flow turbulent flow radius diameter vector direction turn 180 degrees bend arch normal Davidoff Art Courtesy Ashley Davidoff MD 72835.800 72839 72831.800 72845.800 49483b01 |
Pressure is generated by the heart’s cyclic pumping into the aorta, creating an arterial pressure wave that migrates down the aortic tube. The aorta’s ability to recoil in union with the heart’s contractions along with fluctuations in intrathoracic pressure stabilizes the necessary pressure difference for the movement of blood between two points in a tube. Blood’s velocity depends on such a difference as well as the elastic composition of the aortic walls and the shape of its path as it courses towards the upper and lower reaches of the systemic circulation.
 Major Forces Major Forces
A Pump, Elasticity, Peripheral Resistance and a Sump |
| 72839 Davidoff Art Courtesy Ashley Davidoff MD 72835.800 72839 72831.800 72845.800 49483b01 |
Tubular Nature
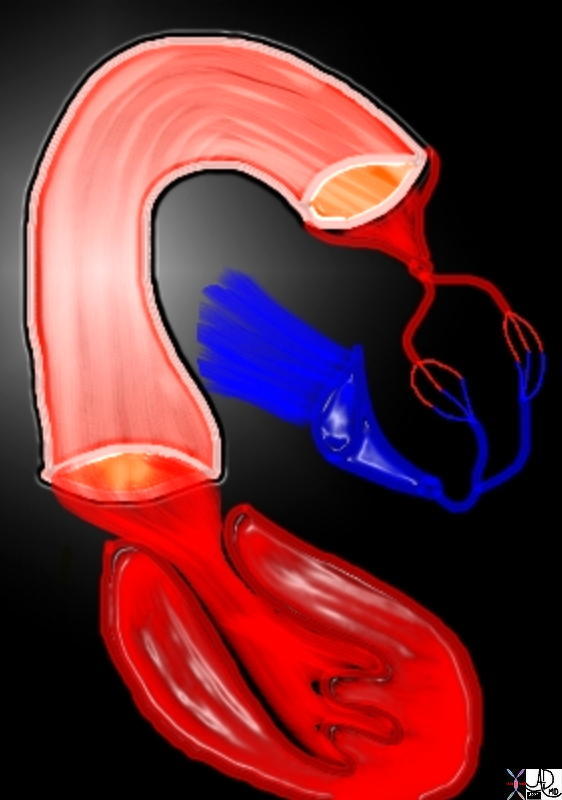
The aorta’s tubular nature executes the transportation of blood throughout the body. Considering the dynamics of tubular blood flow, the aorta’s bent pathway implicates the normally linear flow of blood through a tube. Its curving dimensions create points of flow impact against the tubular walls. At such locations sheer stresses occur and are sometimes the site of dissection and occasionally aneurysmal disease.
 Flow Around the Arch with Locations of Shear Stress Against the Walls Flow Around the Arch with Locations of Shear Stress Against the Walls |
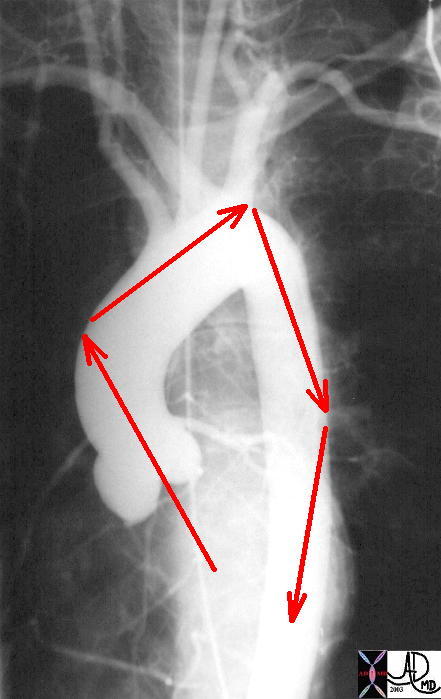
| This normal angiogram of the thoracic aorta shows the areas of shear stress on the aorta. The orientation of the ascending aorta is such that the jet of the LV ejection is directed to the right lateral wall of the aorta. The second region of shear stress is just beyond the left subclavian artery, while the third is at the proximal thoracic aorta. The course thereafter is a straight shot to the bifurcation.
Courtesy Ashley Davidoff MD 27185 01 code CVS artery aorta shear stress |
The aortic arch and abdominal aorta give rise to several large branches, increasing the available sites for flow impact against the walls. This may seem a serious flow issue, but in healthy individuals the effects of shear stress are not of issue. Due to the great muscular strength of the aorta and its viscoelastic properties, the tubular walls are able to withstand the stress caused by axial and transverse collision of blood flow. Its function as a tubular vessel is fulfilled by such properties.
As a tubular conduit, the aorta operates according to the laws that govern blood flow through a tube. When profiling the character of flow through a tube, Reynolds Number is often used. Reynolds number (Re) is a dimensionless quantity that relates the relative importance of inertial forces to viscous forces in fluid mechanics. The ratio can be calculated by integrating the simple formula relating velocity to blood flow, density, viscosity and tubular diameter. When Reynolds number exceeds a certain limit, laminar flow becomes turbulent. Thus the number can be used to predict the type of blood flow present. For the aorta, which has a relatively large diameter and a high rate of pulsatile blood flow, Reynolds number is generally high (approximately 2000-4000). Flow is definitely turbulent in the 5,000 range and definitely laminar below 1000, and is variably laminar in the 1000-5000 range. This would imply that there could be normal turbulent flow in the aorta at peak systole, but in general flow in the aorta and arterial system at large is generally laminar.
Radius and diameter
As blood passes from the ascending to the descending aorta, its pathway narrows as the aorta’s diameter decreases in size from about 3cms. to 2cms. The diameter’s progressive decrease along its course resembles the overall structure of systemic circulation. A diminishing tubular network allows blood to flow everywhere in the body. Blood then experiences increasing effects of fluid friction in addition to the effects from the varying elastic properties of the walls. Its rate of flow must decrease in order for efficient diffusion to occur across the endothelial cell’s permeable membranes. This gives enough time for oxygen to be transported into the adjacent tissues to be converted into metabolic processes.
As a receptacle of cardiac output, the aorta must be large in diameter in order to accommodate the large stroke volume of blood. Diseases which decrease the diameter of the aorta disrupt its receptive ability, causing an increase in flow turbulence as well as an increase in resistance.
Length
In accordance with Poiseulle’s law for laminar flow, the length of a tube is inversely proportional to the velocity of blood flow; the longer the length, the slower the velocity. In general, other factors such as density, viscosity, pressure and diameter have a more relevant effect, all of which vary along the pathway of the aorta. Each portion of the aorta’s course varies in size. Thus blood flow is affected by how long it flows in that particular type of tube or how long the variations in wall structure will influence the nature of blood flow.
Table 1
Relative Sizes of the Vessels of the Vascular System
| diameter mm | length mm | wall thick
mm |
pressure
mmhg |
|
| Arteries | ||||
| aorta | 25 | 400 | 2,000 | 100 |
| large | 6-8 | 200 | 1,000 | 100 |
| medium | 2.5-3 | 100 | 800 | 95 |
| arterioles | .1 | 2 | 20 | 60 |
| Capillaries | .008
(8mm) |
1 | 1 | 30 |
| Veins | ||||
| venules | .15 | 2 | 2 | 20 |
| medium | 5 | 100 | 500 | 15 |
| veins | 14 | 200 | 800 | 10 |
| vena cava | 30 | 400 | 1500 | 0-5 |
| Heart | 120 |
Table 2
Number Length Surface Area and Blood Volume of the Vessels of the Vascular System
| number | length mm | surface area mm2 | blood volume
mms 3 |
|
| Arteries | ||||
| aorta | 1 | 400 | 31,400 | 200,00 |
| large | 40 | 8000 | 163,000 | 260,000 |
| medium | 500 | 50,000 | 377,000 | 220,000 |
| arterioles | 4,500,000 | 9,000,000 | 2,800,000 | 70,000 |
| Capillaries | 19,000,000.000 | 19,000,000.000 | 298,000,000 | 375,000 |
| Veins | ||||
| venules | 10,000,000 | 20,000,000 | 9,400,000 | 355,000 |
| medium | 500 | 50,000 | 785,000 | 1,590,000 |
| veins | 40 | 8,000 | 352,000 | 1,290,000 |
| vena cava | 2 | 400 | 37,700 | 280,000 |
| Heart | 450,000 | |||
| TOTAL | 12,000 miles | 312,900,000 | 5,400,000 |
In the table above the number of capillaries and the length and area covered is astounding .
Shape
As a tube among tubes, the aorta’s curved ascending portion and its arch distinguishes it from the rest. Its design has evolved to incorporate the upward push of blood from ventricular ejection in order to supply blood to the head in addition to the other lower regions of the body. Considering the aorta’s curved geometry in comparison to that of a straight cylindrical tube the aorta experiences collisions with the curving elastic walls. It is the elastic recoil, and overall compliance that in general allows for laminar flow.
As opposed to the peripheral arteries, the aorta has a far greater elastic composition. The stretch and recoil method of the walls converts potential energy into the kinetic energy of blood flow. As blood is pumped against the walls, they simultaneously stretch like a spring. This momentary state stores energy until it is released during diastole by recoiling. This characteristic aids in the progression of blood flow and the gradual dampening of arterial pressure. The thoracic aorta is comprised of a greater amount of elastic tissue (about 56 lamellae) as opposed to the abdominal aorta (only 26 lamellae).
Vessels that are predominately comprised of elastic tissue can transmit pressure waves at a gradual rate by conforming to the pressure deformation as opposed to those predominately comprised of smooth muscle which has lesser compliance and recoil. In an aortic pressure wave curve the dampening effect is apparent as the relatively high-frequency waves become contoured progressively.
As can be seen from the table 3 below, the amount of elastic tissue and fibrous tissue is highest in the aorta while the amount of muscular tissue dominates in the smaller arteries. The amount of elastic tissue is also highest in the proximal aorta and progressively decreases with the least amount in the abdominal aorta. While the capillaries and venules have neither elastic, fibrous nor muscular tissue there is a progressive buildup of all three in the veins and vena cavae.
Table 3
Relative Dominanace of the Elastic, Muscular and Fibrous Tissue in the Walls of the Vascular System Elasticity
| vessel | ratio of lumen
diameter to wall thickness |
diameter | thickness
of wall |
elastic
tissue |
smooth
muscle |
fibrous
tissue |
| aorta | ~ 12:1 | 25 mm | 2 mm | ++++ | ++ | +++ |
| artery | ~ 4:1 | 4 mm | 1 mm | +++ | ++++ | ++ |
| arteriole | ~ 1.5:1 | 0.03 mm
(30mm) |
0.02 mm | ++ | +++ | ++ |
| pre-
capillary sphincter |
~ 1:1 | 0.035mm
(35mm) |
0.030 mm | + | +++ | + |
| capillary | ~ 8:1 | 0.008mm
(8mm) |
0.001 mm | 0 | 0 | 0 |
| venule | ~ 10:1 | 0.020mm
(20mm) |
0.002 mm | 0 | 0 | + |
| vein | ~ 10:1 | 5 mm | 0.5 mm | ++ | ++ | ++ |
| vena
cava |
~ 15:1 | 30 mm | 1.5 mm | ++ | +++ | +++ |
Applied Biology
The abdominal aorta is the most common site for aneurysmal disease which affects about 3-4% of the population.
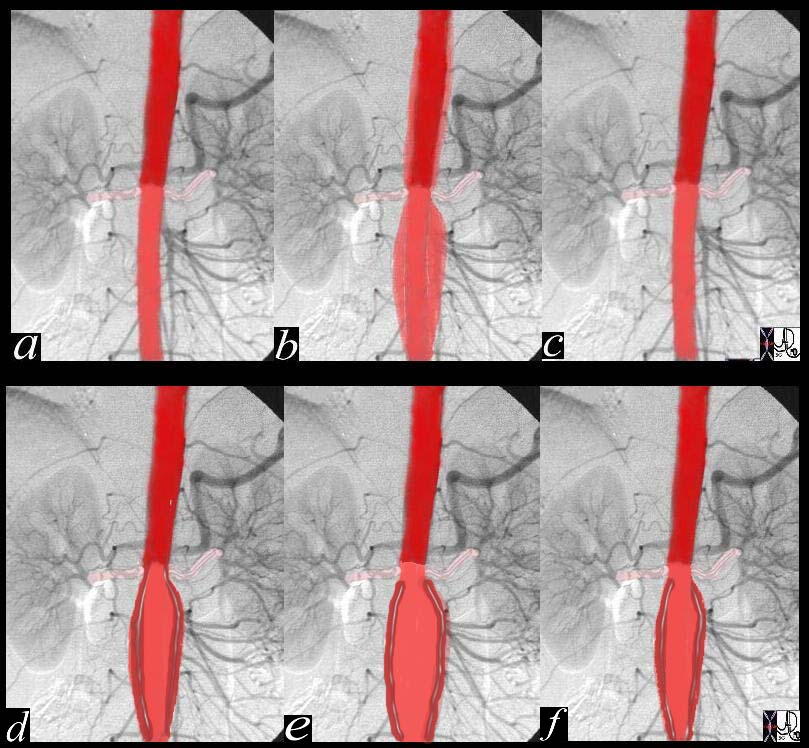 Evolution of Aneurysmal Disease Normal (a,b,c) and Aneurysm (d,e,f) Evolution of Aneurysmal Disease Normal (a,b,c) and Aneurysm (d,e,f) |
| This angiogram with overlay shows a theoretical changes of the aortic wall during diastole (a) systolic expansion (b) and return to normal in diastole (c) In systole (b) the suprarenal artery is expanded by the pulse but is relatively decompressed by the low resistance and high flow renal arteries. The infrarenal aorta is relatively more expanded in systole (b) since the iliac arteries offer a relative resistance. This increased resistance causes the elastic tissue in the aorta to stretch (b) so that the recoil in diastole (c) results in a sustained forward moving force assisting the blood to get to their most distal destination – the feet. When the aorta starts to lose its elasticity the recoil of systole gradually is weakened so that the aorta does not return to its normal diameter after each systolic expansion. Over many years this lack of recoil is progressive so that the resulting wall is weaker and dilated, until an aneurysm is formed. A small infrarenal fusiform aneurysm is seen in images d(diastole), e, (systole) and f, diastole. Some recoil is still present, as seen by a systolic dilatation (e) with slight decrease in diameter during diastole (f).
Courtesy Ashley Davidoff 24877c04 |
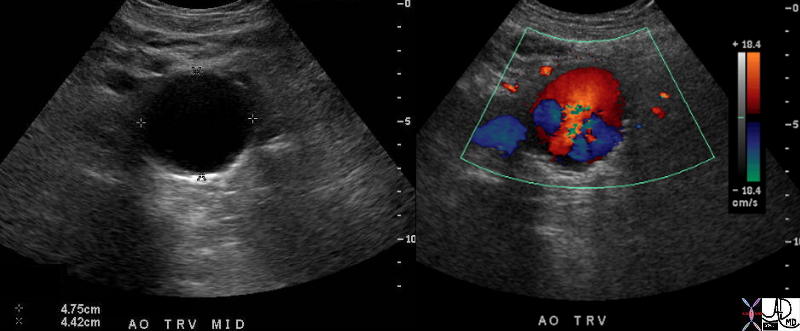 Turbulence in an Abdominal Aortic Aneurysm Turbulence in an Abdominal Aortic Aneurysm |
| 37669c01 aorta abdomen abdominal aort AAA enlarged aneurysm abdominal aortic aneurysm turbulent flow USscan color flow doppler Courtesy Ashley Davidoff MD |
Histology
The high proportion of elastic fibers in the aortic wall allows for its repeated distension and recoil, which damps the effects of ventricular systole (rhythmic upper limit of blood pressure) into smoother but still pulsatile flow through the arterial tree.
The most proximal aorta contains the largest amount of elastic tissue where the recoil function is most critical, and the amount of elastic tissue progressively decreases distally. The thoracic aorta is comprised of a greater amount of elastic tissue (about 56 lamellae) as opposed to the abdominal aorta (only 26 lamellae). As a result, the proximal thoracic aorta has a more prolonged down stroke during diastole as compared to the distal abdominal aorta..
The aortic wall also contains a muscular layer which is innervated by an investing autonomic nervous plexus. The muscle plays a secondary role in the regulation of the recoil phase. Collagen in the aortic wall provides tensile strength and prevents further stretch. The wall of the abdominal aorta is in general thicker than the thoracic aorta due to the higher hydrostatic pressure in the lower regions of the body (below the heart) when the body is erect.
References
Biomechanics – Motion Flow Stress and Growth by Yuen-cheng Fung Fitridge and Thompson MEchanisms of Vascular Disease |
 Histology – Key to Aortic Function is its Elastic Layer (teal)
Histology – Key to Aortic Function is its Elastic Layer (teal)